Prediabetes (impaired fasting glucose or elevated HbA1c short of diabetes) is a reversible metabolic state for many people. With the right combination of diet, physical activity, sleep, and targeted support, progression to type 2 diabetes can often be prevented — and in many cases blood glucose can return to the normal range. This article gives a protocol-style plan with measurable actions, a realistic timeline, and when to seek medical help. Where evidence exists, I cite high-quality reviews and guideline statements so you can see the science behind the steps.
Quick primer: what counts as prediabetes
- Fasting plasma glucose (FPG): 100–125 mg/dL (5.6–6.9 mmol/L)
- 2-hour OGTT: 140–199 mg/dL (7.8–11.0 mmol/L)
- HbA1c: 5.7%–6.4%
(Use whichever test your clinician recommends; having a baseline HbA1c + fasting glucose is ideal.)
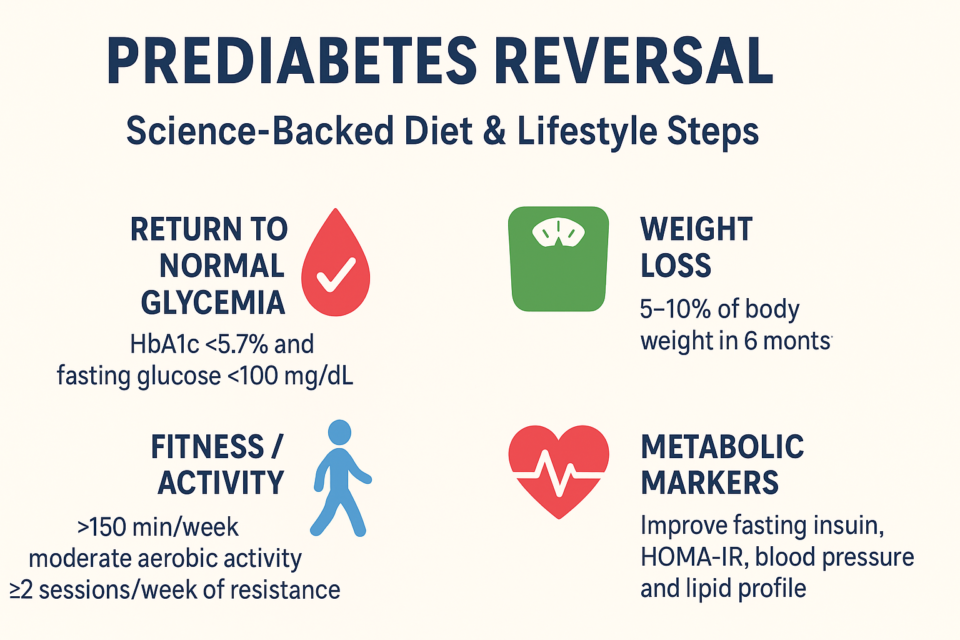
Overarching goals (measurable)
- Return to normal glycemia: HbA1c <5.7% and fasting glucose <100 mg/dL where possible.
- Weight loss: 5–10% body weight within 6 months (higher weight loss yields greater likelihood of normalization).
- Fitness / activity: ≥150 minutes/week moderate aerobic activity plus ≥2 sessions/week of resistance training.
- Metabolic markers: improve fasting insulin/HOMA-IR, blood pressure, and lipid profile.
These targets are supported by diabetes-prevention trials and guideline reviews showing lifestyle changes reduce progression and improve intermediate markers.
The 12-Week Protocol (what to do, day by day / week by week)
This section is a practical protocol you can follow. It’s written so you can apply it immediately and measure progress.
Baseline (week 0 — before you start)
Actions:
- Get labs: Fasting glucose, fasting insulin (optional), HbA1c, lipid panel, ALT, creatinine. Obtain baseline weight, waist circumference, blood pressure.
- Record food intake for 3 days and note typical sleep pattern.
- Discuss with your clinician if you are on glucose-altering medications, pregnant, breastfeeding, or have medical conditions — adjust plan accordingly.
Why: baseline labs let you measure success and identify if medication or specialist referral is needed.
Weeks 1–4: Build the foundation (small, measurable wins)
Daily measurable actions:
- Calories & protein: Aim for a moderate calorie deficit to target 0.5–1.0% body weight loss per week (approx. 500 kcal/day deficit). Aim for 1.2–1.6 g/kg ideal body weight of protein daily to preserve lean mass.
- Meal pattern: Eat within a consistent window (e.g., 10–12 hour window) or use time-restricted eating (TRE) like 10–8 hours if appropriate — TRE can modestly improve fasting glucose and support weight loss. Start with a 12-hour window and shorten gradually.
- Carbohydrate quality: Replace refined carbs with whole-food carbs: vegetables, legumes, intact whole grains, and fruit. Target fiber ≥25–30 g/day. Favor low glycemic index/load choices.
- Physical activity: Walk briskly 30 minutes/day, 5 days/week (150 min/week). Add 2 resistance sessions/week (full-body, 30–40 minutes). Log workouts in an app or notebook.
- Sleep and stress: Aim for 7–9 hours/night and practice a nightly wind-down (no screens 30–60 minutes before bed). Add 10 minutes daily of a stress-reduction practice (breathing, mindfulness).
Weekly measurable tasks:
- Weigh once per week, same morning, same clothes; measure waist circumference every 2 weeks. Record fasting glucose once per week (fasting fingerstick or lab if available).
- Reduce sugary beverages to zero; replace with water, unsweetened tea, or coffee (limit added sugar).
Why these steps:
- Even modest weight loss (5–7%) is associated with large reductions in diabetes risk in prevention programs (Diabetes Prevention Program and real-world translations).
Weeks 5–12: Intensify and personalize
Goals: achieve 5% weight loss by week 12 if possible; improve fitness and dietary consistency.
Actions (progressive):
- Dietary pattern choice: Pick a sustainable, evidence-based pattern: Mediterranean-style (vegetable-heavy, olive oil, nuts, fish, whole grains) or moderate/low-carbohydrate approach if preferred. Both show glycemic benefits; choose one you can sustain. Target 45–50% carbs (Mediterranean/moderate) or <130 g/day for a more carbohydrate-restricted approach — keep total calories in a deficit for weight loss.
- Fiber & volume: Prioritize non-starchy vegetables, legumes, and whole fruits. Aim for ≥30 g fiber/day to slow glucose absorption and support microbiome diversity.
- Protein & strength training: Keep protein high to preserve muscle during weight loss. Progress resistance training intensity (e.g., increase weight or reps every 2 weeks). Resistance training improves glucose metabolism independent of weight loss.
- Cardio progression: Add 1–2 higher-intensity intervals per week if able (e.g., 2 min faster walk/jog x 6 repeats within your 30–40 min session).
- Monitor: Check fasting glucose weekly and HbA1c at 3 months (or sooner if clinically indicated). Expect modest reductions in fasting glucose during this window if you keep weight loss and activity consistent.
Maintenance and remission phase (3–12 months)
Actions:
- If fasting glucose and HbA1c return to normal, shift to maintenance calories and keep activity levels. Sustained weight loss is the strongest predictor of lasting normoglycemia.
- Continue regular resistance training and 150+ min/week activity.
- If glycemia remains in the prediabetes range despite adherence, discuss adjuncts with your clinician (see “When medication may be considered” below).
Evidence summary: lifestyle programs modeled after the DPP reduce progression to diabetes by ~58% over 3 years; even pragmatic lower-intensity programs produce meaningful risk reduction.
Specific diet options — practical details (pick one and personalize)
1) Mediterranean-style moderate-carb plan (sustainable, heart-healthy)
- Calories: 10–20% deficit to start.
- Plate rule: ½ non-starchy vegetables, ¼ lean protein, ¼ whole grains/legumes.
- Daily: olive oil (2 tbsp), 2–3 servings fatty fish/week, nuts 1 small handful, limited added sugar.
- Why: improves insulin sensitivity, lipids, and reduces diabetes risk in trials when combined with weight loss.
2) Moderate/low-carbohydrate (for people who tolerate lower carbs)
- Carbs: 50–130 g/day (personalize).
- Focus on non-starchy vegetables, legumes, whole fruit in moderation, and lean protein.
- Monitor ketone symptoms if you go very low carb and discuss with clinician. Evidence shows low-carb can improve glycemia and support weight loss, but long-term adherence is key.
3) Time-restricted eating (circadian-aligned)
- Example: 10-hour feeding window (10:00–20:00) or 8-hour (12:00–20:00) if tolerated.
- Do not binge — quality still matters. TRE can amplify weight loss and reduce fasting glucose in short trials. Use only if it suits your lifestyle and you have no contraindications.
Exercise plan (practical, measurable)
- Aerobic: 150 minutes/week moderate (e.g., brisk walking 30 min ×5) OR 75 min vigorous.
- Resistance: 2–3 sessions/week, 6–8 exercises covering major muscle groups, 2–3 sets of 8–12 reps. Increase load progressively.
- Optional: Add flexibility/balance or high-intensity intervals as tolerated.
- Rationale: Aerobic + resistance improves glucose disposal and insulin sensitivity; resistance training has independent benefits.
Monitoring and measurable milestones
- Weekly: weight, fasting glucose (fingerstick or lab), step count, exercise minutes.
- Every 3 months: HbA1c, lipid panel, BP, waist circumference.
- Milestones:
- 1 month: 1–3% weight loss, small fasting glucose improvement.
- 3 months: aim for ≥5% weight loss; lower fasting glucose and improved lipids likely.
- 6–12 months: 5–10% (or more) weight loss — highest chance of normalizing glucose.
Tools & tracking (concrete)
- Food app (MyFitnessPal, Cronometer) to track calories/macros.
- Activity tracker or phone step counter. Goal: 7,000–10,000 steps/day plus exercise sessions.
- Weight scale and tape measure for waist.
- Blood glucose monitor for fasting checks (or home A1c kits if available).
- Optional: continuous glucose monitor (CGM) for detailed patterns (discuss with clinician/insurer).
When to consider medication or specialty referral
- If glycemia worsens toward diabetes (HbA1c ≥6.5% or fasting glucose ≥126 mg/dL or 2-hr OGTT ≥200 mg/dL), start diabetes workup and discuss medication.
- Metformin has evidence to reduce progression to diabetes in higher-risk prediabetes individuals (younger, higher BMI, history of gestational diabetes) and is recommended selectively by guideline panels; discuss with your clinician.
- For those with obesity and severe metabolic disease, referral for anti-obesity medications or bariatric/metabolic surgery may be appropriate after specialist assessment — these options can induce diabetes remission in many cases but require specialist care.
Troubleshooting (common barriers & fixes)
- Plateau in weight loss: re-check calorie intake, increase resistance training intensity, reduce liquid calories, and ensure sleep ≥7 hours.
- Hunger on calorie deficit: increase protein + fiber (vegetables, legumes), schedule high-volume low-calorie meals (salads, broths).
- Low motivation: join structured programs (DPP-based classes), find an exercise buddy, use telehealth/digital coaching. Even lower-intensity program translations of DPP yield benefit.
Safety and special populations
- Pregnant or breastfeeding people, those with eating disorder history, or certain medical conditions should not start aggressive caloric restriction or fasting without medical oversight.
- If you are on glucose-lowering medications, monitor closely for hypoglycemia as you lose weight and increase activity; medication adjustments may be needed.
Sample 1-day menu (Mediterranean style, ~1,600 kcal example)
- Breakfast: Greek yogurt (plain) with berries, 1 tbsp chopped nuts, and flaxseed.
- Snack: Apple + 1 tbsp almond butter.
- Lunch: Large salad (mixed greens, chickpeas, cherry tomatoes, cucumber), 3 oz grilled chicken, 1 tbsp olive oil + lemon dressing, small whole-grain pita.
- Snack: Carrot sticks + hummus.
- Dinner: Baked salmon (4 oz), steamed broccoli, ½ cup quinoa.
- Beverage: water/tea; no sugar.
Adjust portions to your calorie target.
What the evidence says (short summary of load-bearing findings)
- Lifestyle interventions (structured diet + activity programs modeled on the Diabetes Prevention Program) reduce progression from prediabetes to type 2 diabetes substantially and are the first-line approach.
- Weight loss is the single strongest predictor of returning to normal glycemia — modest loss (5–10%) yields meaningful benefit.
- Diet quality matters: Mediterranean and lower-carbohydrate diets both show benefits for glycemic control; choose the pattern you can follow long term.
- Exercise: combining aerobic and resistance training is effective; resistance training has benefits independent of weight loss.
- Time-restricted eating shows promise for modest fasting glucose improvements and weight loss in recent studies; more long-term data are emerging.
Short FAQ (for SEO snippets)
Q: Can prediabetes be reversed?
A: Yes—many people return to normal glycemia with sustained lifestyle changes (weight loss, diet quality, exercise), though individual results vary.
Q: How fast will I see results?
A: Some fasting glucose improvements occur within weeks; measurable HbA1c changes are best assessed at 3 months. Aim for 1–2 lbs/week weight loss initially.
Q: Is medication ever recommended?
A: Medication like metformin may be considered for high-risk individuals in addition to lifestyle changes; discuss with your clinician.
Final note — realistic expectations & momentum
Reversing prediabetes is not a single “hack” — it’s a set of sustainable habits that together change body composition, insulin sensitivity, and metabolic health. Structured programs (DPP or similar) produce the strongest evidence, but even pragmatic, personalized approaches (Mediterranean pattern, resistance + aerobic training, and consistent sleep) produce meaningful gains. Start with small, measurable steps this week (weigh, baseline labs, 3 days food log, 3 brisk walks), and build toward the 12-week protocol above.
Sources
- Jonas DE, et al. Screening for Prediabetes and Type 2 Diabetes. JAMA/USPSTF summary and evidence review (2021). PubMed
- American Diabetes Association / Diabetes Care — Prevention recommendations and lifestyle program evidence (Diabetes Care supplement 2025). Diabetes Journals
- Jing T., et al. “Effect of Dietary Approaches on Glycemic Control” Nutrients (2023). MDPI
- Luo X., et al. “Effect of resistance vs. aerobic exercise in pre-diabetes” (2023). PubMed
- Wong P., et al. Meta-analysis on 16/8 time-restricted eating and glucose metabolism (2025). OUP Academic
- Tseng E., et al. Systematic review: Lower-intensity lifestyle interventions for prediabetes (2023). PMC
- Griauzde D.H., et al. Low-carbohydrate adaptations of DPP feasibility trial (BMJ Open, 2020). BMJ Open
- USPSTF recommendation on screening and comment on metformin effectiveness (2021). USPSTF+1